How does a normal bladder work?
The bladder is a hollow organ in the lower abdomen. It stores urine; the liquid waste produced by the kidneys. Urine
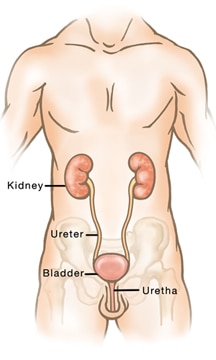
passes from each kidney into the bladder through a tube called a ureter. Urine leaves the bladder and exits the body through another tube called the urethra.
As the bladder fills with urine, pressure is exerted on its walls, which you experience as the need to urinate. This triggers the brain to send a message to the layer of muscle that surrounds the inner lining of the bladder, forcing the muscle to contract (tighten) and the urine to flow out of the bladder.
At the same time, the sphincter muscle that surrounds the urethra relaxes, letting the urine flow out of the body. This process requires both nerves and muscles working together to prevent urine leakage. Damage, weakening or injury to either muscles or nerves can result in incontinence.
Are you showing signs of incontinence?
Below are some simple questions to think about before talking to your doctor:
Do you leak urine unexpectedly?
Yes
No
How much do you leak?
A few drops
Wet undergarments
Wet clothing
Do you leak urine when you:
Cough?
Sneeze?
Laugh?
Bend?
Lift?
Change positions (i.e., sitting or laying to standing)?
Do you leak urine continuously during the day?
Yes
No
Do you leak urine while sleeping?
Yes
No
Does urine leakage affect your life?
Yes
No
If you answered yes to any of these questions or if you think incontinence is preventing you from enjoying life, talk to your doctor. They can diagnose your type of incontinence and help you find the most effective treatment option.